Abstract

Challenges in the East Mediterranean Region (EMR) Policy Brief / Report-ready Executive Summary
The East Mediterranean Region (EMR) spans 22 countries and over 700 million people, facing a convergence of protracted conflict and displacement, health system fragility, a double burden of disease, climate and environmental stressors, and widening socioeconomic inequities. This overview synthesizes key problem domains and priority pathways to strengthen regional health security, equity, and resilience.
1. Introduction 2. Conflict & Displacement 3. Health Systems & Workforce 4. Double Burden of Disease 5. Environment & Climate 6. Inequities & Governance 7. Mental Health 8. Pathways Forward 9. Conclusion 1) IntroductionThe EMR from Morocco and Sudan to Pakistan and Afghanistan encompasses diverse economies and health capacities. Recurrent crises, displacement, and economic shocks have deepened vulnerability and disrupted essential services. The result is an uneven landscape of health outcomes, underfunded public systems, and dependencies on humanitarian mechanisms amid chronic instability.
2) Conflict, Displacement, and Humanitarian CrisesProtracted conflicts (e.g., Syria, Yemen, Sudan, Palestine, Afghanistan, Somalia) have displaced millions internally and across borders. Overcrowded settings with limited WASH infrastructure drive outbreaks (cholera, measles, TB) and interrupt immunization and maternal services. Surveillance and routine care falter, increasing excess mortality and long-term disability. Humanitarian access constraints and attacks on health care further degrade service continuity.
3) Health System Fragility and Workforce ShortagesMany EMR countries invest below 5% of GDP in health, yielding outdated facilities, supply chain gaps, and inadequate digital infrastructure. Workforce migration driven by insecurity and poor remuneration—creates chronic shortages, especially in rural and conflict-affected areas. Essential programs for maternal–child health, NCDs, and mental health remain under-resourced, while COVID-19 exposed limitations in preparedness, laboratory networks, and data systems.
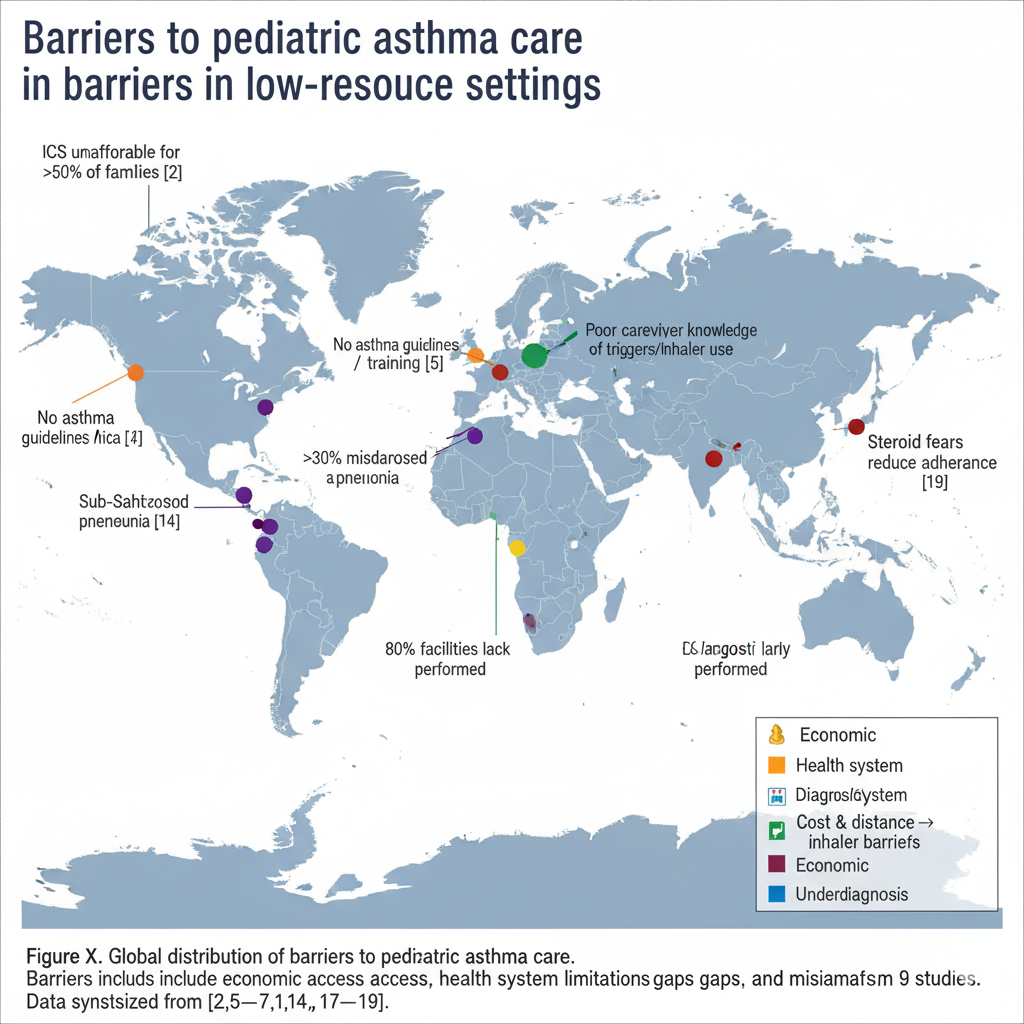
4) The Double Burden of DiseaseCommunicable diseases remain endemic where vaccination and surveillance are disrupted, while non-communicable diseases (cardiovascular disease, diabetes, cancers, chronic respiratory disease) account for a growing majority of deaths. Tobacco use, unhealthy diets, and physical inactivity amplify NCD risk. Rapid urbanization and economic transitions accelerate obesity and metabolic disorders, straining already fragile systems.
5) Environmental and Climate-Related ChallengesHeat stress, drought, and water scarcity threaten food security and livelihoods. Major urban centers experience hazardous air pollution far above WHO guidelines, increasing respiratory and cardiovascular risk. Desertification and extre

