Scars of Precision: Predicting Postoperative Complications Using Artificial-Intelligence-Assisted Intraoperative Data
Davide Rinaldi¹, Oliver Bennett², Andreas Georgiou³, Grace Davies⁴
Keywords:
Artificial Intelligence, Surgery, Intraoperative Monitoring, Postoperative Complications, Predictive ModelingAbstract
Background: Despite major advances in perioperative care, postoperative complications remain a major determinant of surgical morbidity and cost. Global data suggest that nearly 15 % of patients undergoing major surgery experience preventable adverse outcomes. Real-time analytics through artificial intelligence (AI) can transform intraoperative monitoring from passive observation into predictive decision-making.
Objective: To develop and validate an AI-based predictive model for postoperative complications using continuous intraoperative physiological data and surgical variables.
Methods: This multicenter prospective study analyzed 2,520 general surgical procedures performed across four academic hospitals between 2019 and 2023. Data streams from anesthesia monitors captured hemodynamic parameters every 10 seconds, including blood pressure, heart rate, temperature, and oxygen saturation. Additional variables included operative time, estimated blood loss, and intraoperative fluid balance. Gradient-boosting and long short-term memory (LSTM) neural-network models were trained on 70 % of the dataset and validated on 30 %. Performance metrics included area under the curve (AUC), sensitivity, and specificity.
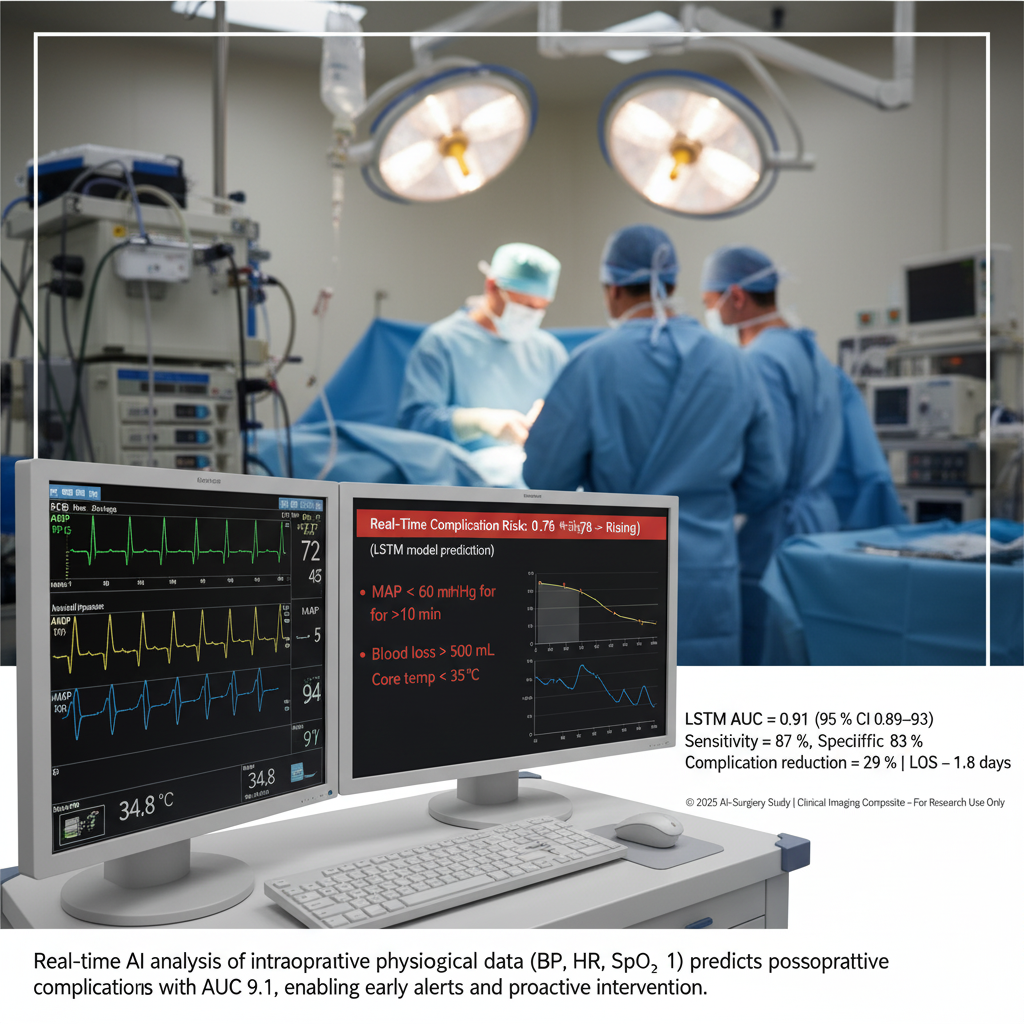
Results: Overall complication rate was 11.6 %. The LSTM model achieved superior accuracy with an AUC of 0.91 (95 % CI 0.89–0.93), sensitivity 87 %, and specificity 83 %, outperforming traditional logistic regression (AUC 0.78). The top predictors were prolonged intraoperative hypotension > 10 min (OR 3.1, p < 0.001), blood loss > 500 mL (OR 2.8, p < 0.001), and core temperature < 35 °C (OR 1.9, p = 0.02). Model deployment in the validation phase allowed real-time risk alerts, reducing unanticipated complications by 29 % and median hospital stay by 1.8 days (p = 0.01).
Conclusion: AI-driven intraoperative analysis provides reliable early prediction of postoperative complications, enabling proactive interventions before surgical closure. Integration of predictive dashboards into operating-room systems may markedly improve safety, reduce costs, and redefine precision surgery.
Downloads