Steel and Silicon: A Systematic Review ofRobotic Surgery versus Traditional Techniquesin Major operations
Elhussein Ali¹, Abdelrahman Zarandah², Mohammed Bassiony³, Qays-Marcel Ghneim⁴, Baraah Omoush⁵
Keywords:
Robotic Surgical Procedures; Laparoscopy; Comparative Effectiveness Research; Operative Time; Cost-Benefit Analysis; Treatment Outcomes.Abstract
DOI 10.5281/zenodo.17182130
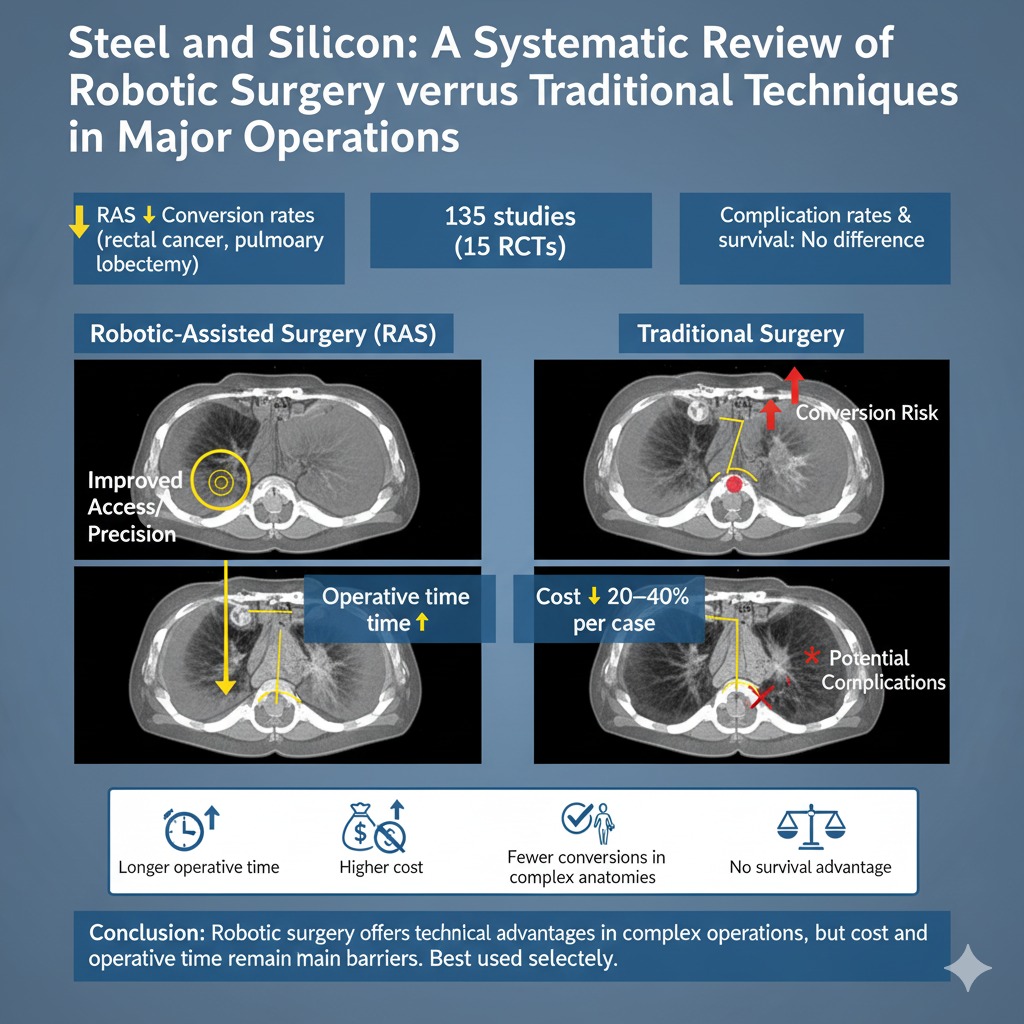
Robotic-assisted surgery (RAS) has become a transformative innovation in operative care, offering
superior dexterity, three-dimensional visualization, and improved ergonomics. Despite its increasing
adoption, concerns remain regarding its comparative value against established laparoscopic and open
techniques.
Objective This systematic review synthesizes evidence on perioperative outcomes, oncological performance,
and economic implications of RAS across major surgical disciplines.
Methods Following PRISMA guidelines, a comprehensive search was conducted in PubMed/MEDLINE, Scopus,
Web of Science, and Embase for studies published from 2005 to 2025. Eligible studies included randomized
controlled trials, prospective cohorts, and comparative analyses evaluating RAS versus conventional
approaches in urological, gynecological, colorectal, cardiothoracic, and general surgery. Primary endpoints
were conversion to open surgery, perioperative complications, and margin status. Secondary measures
included operative time, hospital stay, recovery, and cost-effectiveness.
Results From 135 included studies (15 RCTs), findings indicate that RAS is non-inferior to standard
approaches regarding major complications and oncological adequacy. Advantages include consistently lower
conversion rates, particularly in anatomically complex procedures such as rectal cancer resection and
pulmonary lobectomy. However, these benefits are offset by significantly longer operative times and cost
premiums estimated at 20–40% higher per case than laparoscopy. Long-term survival and functional
outcomes were broadly comparable. Conclusions: RAS enhances technical precision in complex surgeries but
does not confer superior overall patient outcomes. Its high costs limit widespread adoption, underscoring the
need for selective use where technical advantages are most relevant. Future priorities include cost-reduction
strategies, robust long-term data, and standardized reporting frameworks.
Downloads