Anti-VEGF Therapy for Diabetic Macular Edema: A Systematic Review and Meta-Analysis
Khadeiga Kononna¹*, Amna Elbasheer¹*, Rofida Mohammed², Sally Muhamed³, Abla Yousif⁴
Keywords:
Diabetic Macular Edema; Anti-VEGF Therapy; Aflibercept; Ranibizumab; Bevacizumab; Visual AcuityAbstract
Corresponding Author : *Amna Elbasheer
Background: Diabetic macular edema (DME) remains a leading cause of visual impairment worldwide. Anti-vascular endothelial growth factor (anti-VEGF) agents—including ranibizumab, aflibercept, and bevacizumab—have emerged as standard treatments. However, uncertainties persist regarding their comparative efficacy, optimal dosing schedules, safety profiles, and cost-effectiveness.
Methods: This systematic review and meta-analysis included 25 studies published between 2005 and 2025, comprising 20 randomized controlled trials and 5 observational studies. The primary outcomes assessed were best-corrected visual acuity (BCVA), central retinal thickness (CRT), safety events, and economic impact. Data were pooled using a random-effects model, accounting for heterogeneity with an I² threshold above 50%.
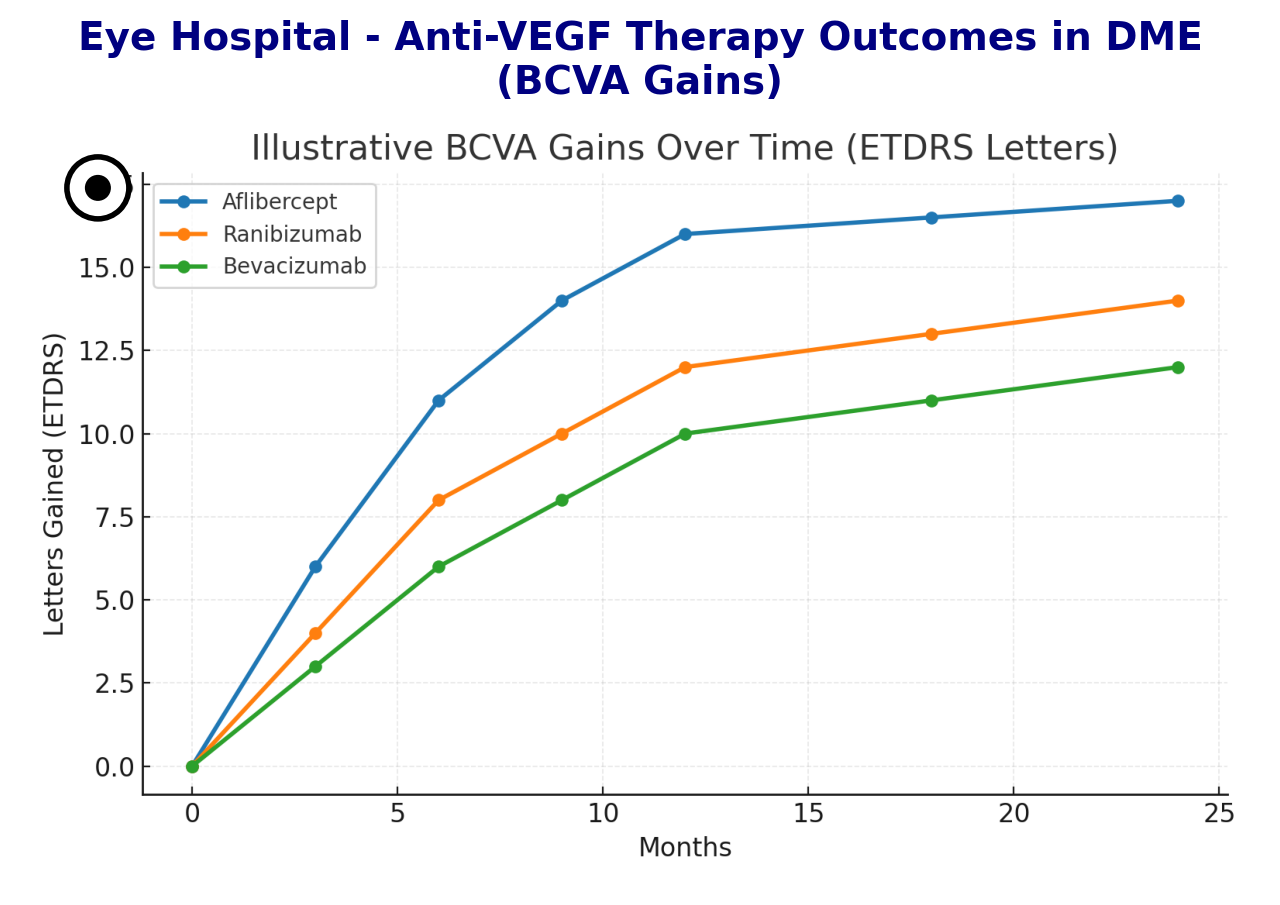
Results: Anti-VEGF therapy consistently produced meaningful improvements in visual function and anatomical outcomes. Aflibercept showed the highest efficacy, with BCVA gains ranging from +13.1 to +17.1 ETDRS letters, particularly benefiting patients with baseline visual acuity of ≤20/50 or <69 letters. Ranibizumab achieved improvements between +5.9 and +14.0 letters, while bevacizumab yielded gains from +4.9 to +12.1 letters, with better outcomes observed in patients with less severe vision loss. Central retinal thickness reductions followed a similar hierarchy: aflibercept led to a mean reduction of approximately −171 µm, ranibizumab between −119 and −194 µm, and bevacizumab from −42 to −126 µm. Regarding treatment protocols, monthly and pro re nata (PRN) regimens were both effective. However, treat-and-extend protocols notably reduced injection frequency after the first year while maintaining efficacy.
All three agents demonstrated a favorable safety profile. Serious adverse events were rare and included endophthalmitis (0.05–0.1%), arterial thromboembolic events (≤1%), transient elevations in intraocular pressure, and conjunctival hemorrhage. Bevacizumab emerged as the most cost-effective option, particularly for patients with milder disease severity, while aflibercept remained the agent of choice in cases requiring maximal therapeutic effect despite its higher cost.
Conclusion: Anti-VEGF therapy offers robust improvements in both visual acuity and retinal anatomy for patients with DME. Aflibercept provides the greatest benefit in more severe cases, whereas bevacizumab offers a practical and cost-effective alternative. Treat-and-extend regimens represent a promising approach to reduce treatment burden without compromising efficacy. Future studies should focus on long-term safety outcomes, personalized treatment strategies, and innovative drug delivery systems to improve adherence and outcomes.
Downloads