Subclinical Biomarkers for Early Neurodegenerative Disease Detection: A Systematic Review
Ahmed Abdalla¹, Abdulwahhab Al-Shaikhli², Abdelrahman Zarandah³, Qays-Marcel Ghneim⁴, Bara Elhadi Diafalla Elmana⁵
Keywords:
Subclinical biomarkers, neurodegeneration, plasma p-tau217, neurofilament light chain (NfL), Alzheimer’s disease, early detection, predictive performanceAbstract
Doi : 10.5281/zenodo.17218654
Neurodegenerative diseases (NDs) such as Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS), impose a growing global burden, yet diagnoses often occur late when therapeutic options are limited. Subclinical biomarkers detectable in cognitively unimpaired individuals may enable earlier detection and intervention.
Objectives: This systematic review assessed the predictive performance of cerebrospinal fluid (CSF), plasma, imaging, and omics-based biomarkers in preclinical neurodegeneration.
Methods: Following PRISMA 2020 guidelines, 25 longitudinal and nested case–control studies published between 2000 and 2025 were included, encompassing more than 100,000 participants. Cohorts were drawn primarily from the United States (56%) and Sweden (24%), with follow-up durations ranging from 2 to 30 years.
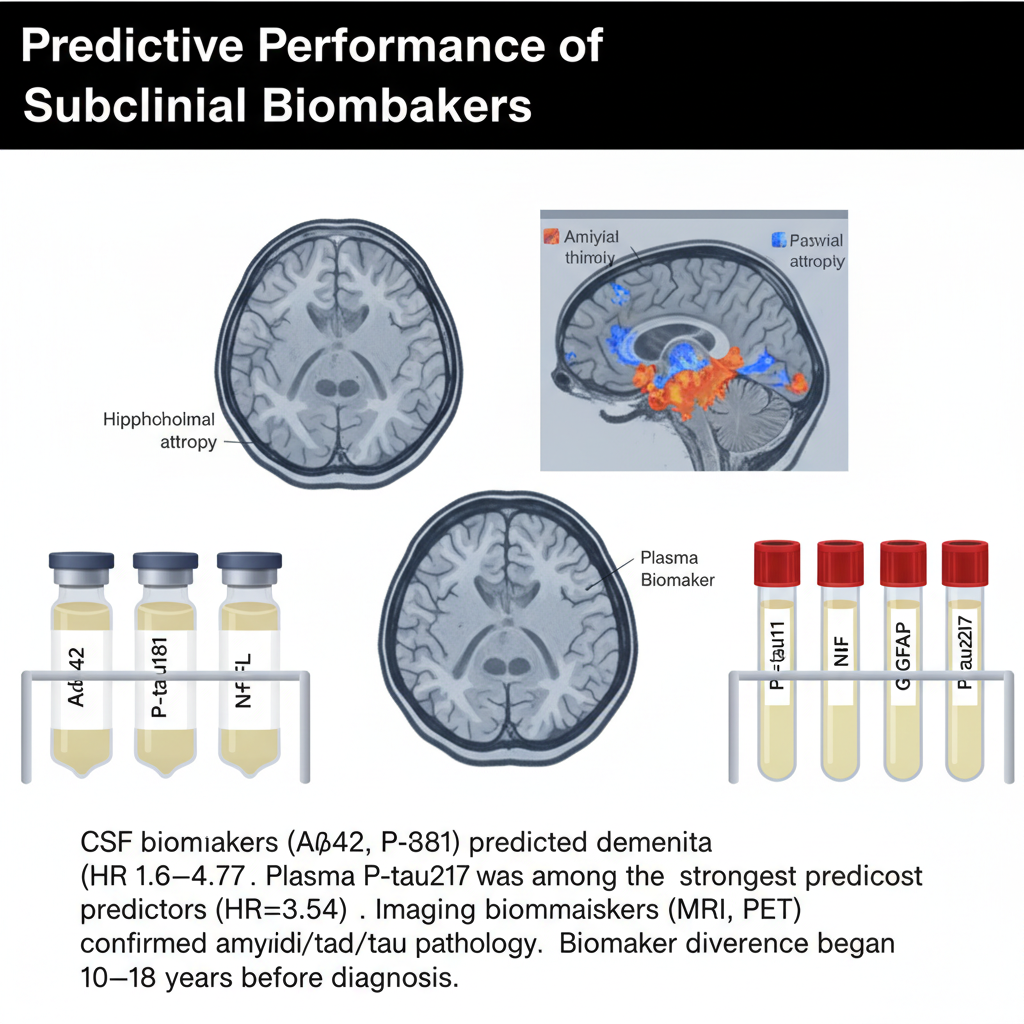
Results: Biomarker abnormalities consistently preceded clinical onset by more than a decade. CSF markers including NfL, Aβ42, and P-tau181 predicted dementia with hazard ratios (HRs) of 1.6–4.77 and prediction windows of up to 20 years. Plasma biomarkers showed strong prognostic performance: P-tau181 (HR=1.15; 95% CI: 1.06–1.25), NfL (HR=1.92; 95% CI: 1.72–2.14), and GFAP (HR=2.35; 95% CI: 1.22–4.53) predicted dementia over 6–24 years, while plasma P-tau217 emerged as the most specific AD marker (HR=3.54; p<0.0001). Imaging biomarkers confirmed pathology, with amyloid PET predicting impairment at HR=10.36 and MRI volumetric analyses achieving AUCs up to 0.95. Temporal trajectories showed Aβ and tau divergence 10–18 years pre-diagnosis, followed by NfL at ~11 years and neuroinflammatory markers later. Combining plasma Aβ42/40, P-tau, and NfL improved predictive accuracy (AUC 70.9–82.6%) and reduced trial sample sizes by up to 30%. Beyond AD, serum NfL predicted PD (OR=2.54) and plasma NfL was elevated up to 5 years before ALS (RR=2.68).
Conclusions: Subclinical biomarker abnormalities are robust predictors of neurodegeneration detectable long before symptoms, with plasma P-tau217, CSF NfL, and multimodal biomarker panels showing greatest clinical promise.
Downloads