Are Normal Vitals Misleading? A Systematic Review of Physiological Stability in Patients with Undetected Clinical Deterioration
Mudathir Elyas¹, Magid Abdelrahman², Samah Ahmed³, Amani Ali⁴, Abdelrahman Ali⁵
Keywords:
Normal vital signs; Occult hypoperfusion; Clinical deterioration; Lactate; Continuous monitoring; Early warning scores; Systematic reviewAbstract
Background:
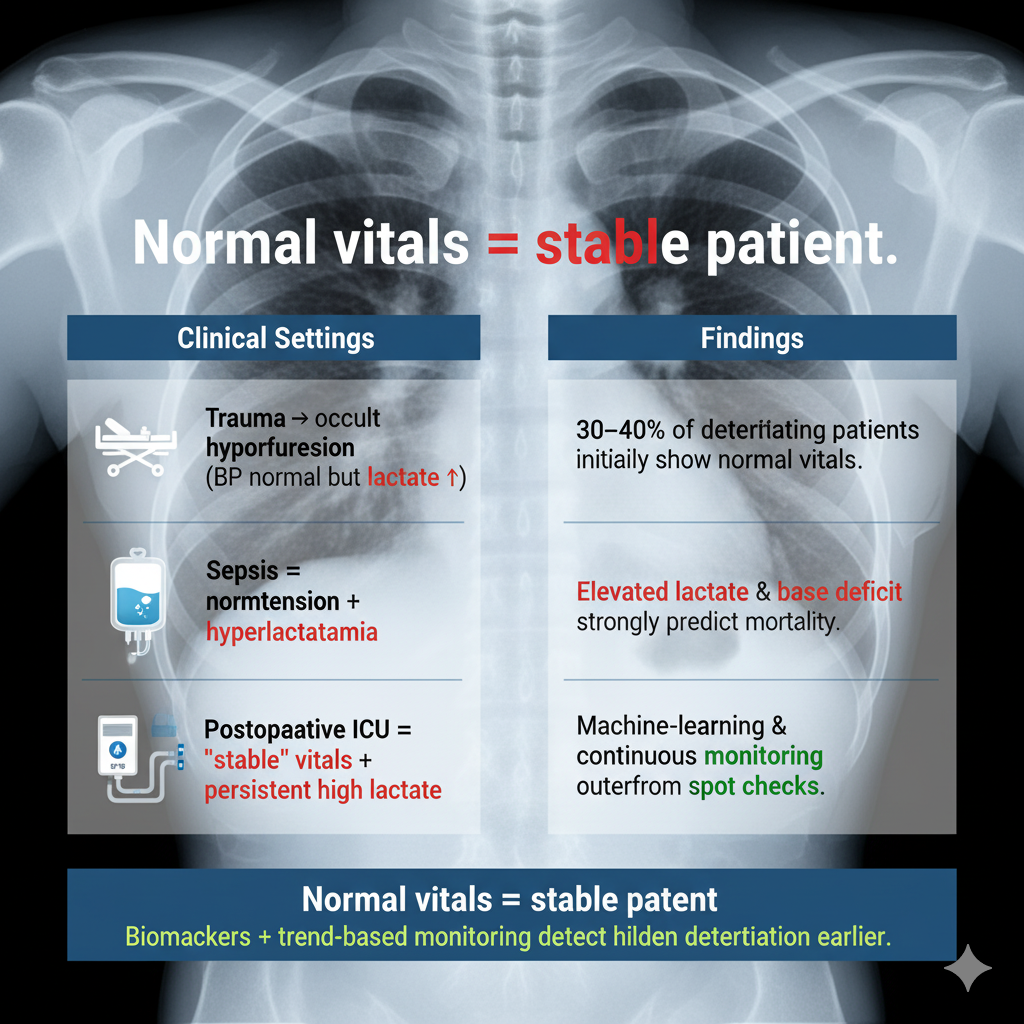
Normal vital signs are often considered reassuring, yet a significant proportion of hospitalized patients experience clinical deterioration despite apparently stable physiology. This phenomenon, termed occult deterioration or occult hypoperfusion, can delay recognition and treatment, leading to preventable morbidity and mortality.
Objective: To systematically review the prevalence, characteristics, and outcomes of adult patients who deteriorate despite presenting with normal vital signs, and to evaluate adjunctive tools such as biomarkers, continuous monitoring, and predictive analytics.
Methods: Following PRISMA 2020 guidelines, we searched PubMed, Scopus, Web of Science, and Google Scholar from January 2000 to March 2025. Eligible studies included observational cohorts, retrospective analyses, and case series (≥10 patients) involving adults (≥18 years) with initial normal vital signs who subsequently deteriorated (ICU transfer, cardiac arrest, or death). Risk of bias was assessed with the Newcastle–Ottawa Scale. Data were narratively synthesized due to heterogeneity.
Results: Twenty-seven studies (sample sizes 44–20,000+) were included, covering trauma, sepsis, surgical, and ICU populations. Across settings, 30–40% of patients who deteriorated had normal vital signs at presentation. Trauma cohorts revealed occult hypoperfusion detectable only by lactate or base deficit, strongly predicting mortality. In sepsis, normotensive patients with elevated lactate had significantly higher mortality compared with normolactatemic peers. Post-operative and ICU studies showed poor outcomes despite stable hemodynamics when hyperlactatemia persisted. Continuous monitoring and predictive analytics demonstrated earlier recognition than intermittent checks, though alarm fatigue remained a limitation.
Conclusion: Normal vital signs do not guarantee physiological stability. A substantial minority of patients at risk for adverse outcomes present with “normal” values, particularly in trauma and sepsis. Adjunctive biochemical markers, trend-based monitoring, and predictive models enhance early detection and should complement conventional vital sign assessment to improve patient outcomes.
Downloads