The Cost of Coordination: Hidden System Failures in Pediatric Referral Pathways Across Emergency Networks
Mia Hoffmann¹, Felix Wagner², James Whitaker³, Emily Clarke⁴
Keywords:
Pediatric Referral, Emergency Coordination, System Failure, Quality of Care, Health ServicesAbstract
Background:
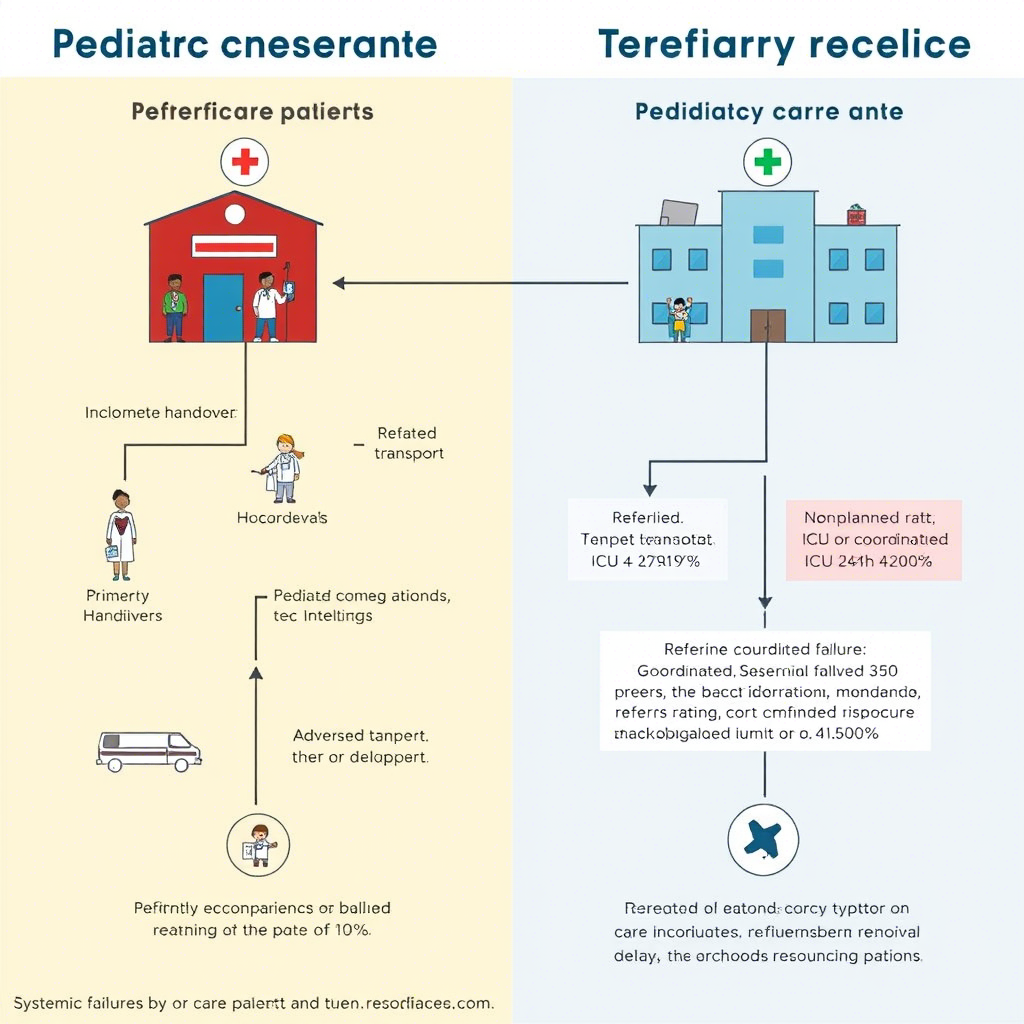
Emergency referral pathways for pediatric patients are designed to optimise time-sensitive care. However, in fragmented health systems, coordination gaps may lead to avoidable delays, duplication of care, or adverse outcomes, often unrecorded in traditional audits.
Objective:
To assess the prevalence and impact of system-level coordination failures in pediatric referrals between primary emergency units and tertiary care hospitals.
Methods:
A retrospective systems audit was conducted across 12 emergency units and five referral hospitals in Germany from February 2022 to January 2024. A random sample of 684 pediatric referrals was analysed using a structured failure taxonomy to identify issues in communication, triage alignment, transport timing, and documentation. The primary outcome was a care delay of more than 2 hours. Secondary outcomes included ED re-evaluation and repeat diagnostics.
Results:
System-level failures were identified in 41.3% of referrals. The most common issues included incomplete handover (23.5%), mismatched triage severity (19.7%), and delayed transport dispatch (12.1%). Delayed care (defined as care received more than 2 hours after the scheduled time) occurred in 35.2% of failure cases, compared to 11.6% in fully coordinated referrals (p < 0.001). Repeat diagnostics were performed in 48.7% of cases with communication lapses. The adjusted odds ratio for adverse events (e.g., unplanned ICU admission) was 2.7 (95% CI: 1.9–4.1) in poorly coordinated referrals.
Conclusion:
Systemic weaknesses in referral coordination remain an underdiagnosed contributor to pediatric emergency inefficiencies. A standardised inter-hospital communication protocol, combined with real-time referral dashboards, could drastically improve outcomes and reduce redundant care. Quality improvement frameworks should consider coordination metrics as key performance indicators.
Downloads